Epilepsy Centers of Excellence (ECoE)
Epilepsy - Symptoms, Causes, Treatments & More

What is epilepsy?
What are seizures?
Epilepsy vs seizures?
First Aid
What are some of the causes of epilepsy?
How is epilepsy diagnosed?
How is epilepsy treated?
What is an electroencephalography (EEG)?
What is Magnetic Resonance Imaging (MRI)?
What is a Positron Emission Tomography (PET) scan?
What is Video EEG Telemetry?
What is Magnetoencephalography (MEG)?
About Pre-surgical Evaluation for Epilepsy.
What is Invasive Monitoring?
What is epilepsy?
Epilepsy is a medical condition that produces seizures that affect a variety of mental and physical functions. When a person has two or more seizures, they are considered to have epilepsy. These seizures are a result of sudden abnormal electrical activity in the brain. The exact type of seizure will depend on where it starts and then spreads within the brain.
What are seizures?
A seizure is a disturbance in the normal regulation pattern of the electrical activity of the brain. Although there are many causes and types of seizures, the common feature is a spreading wave of uncontrolled electrical activity. This abnormal activity within the brain will usually create outward changes in the person experiencing a seizure. Signs and symptoms may include muscle spasms, mental confusion, loss of consciousness and/or uncontrolled or aimless body movements. In general, seizures last a finite period of seconds to minutes, and then stop on their own.
There are two main types of seizures:
Generalized seizures begin with sudden abnormal electrical activity throughout the entire brain at once. These seizure types include: tonic-clonic convulsions ("grand mal" seizures) and absence seizures ("petit mal" or staring seizures).
Partial seizures begin with abnormal electrical activity in just one part of the brain. Although the activity starts in a specific area of the brain, this activity can spread to other parts as well. These seizures types include: simple partial seizures, complex partial seizures, and secondarily generalized seizures.
Epilepsy vs seizures?
Seizures are characterized by a sudden change in movement, behavior, sensation or consciousness produced by an abnormal electrical discharge in the brain. Epilepsy is a condition of spontaneously recurring seizures. Having a single seizure does not necessarily mean a person has epilepsy. High fever, severe head injury, lack of oxygen, or a number of other factors can cause a single seizure.
Epilepsy, on the other hand, tends to be a lifelong condition that affects how electrical energy and connections behave in the brain.
First Aid
Convulsive seizures
- When providing seizure first aid for generalized tonic-clonic (grand mal) seizures or partial seizures with secondary generalization, these are the key things to remember:
- Keep calm and reassure other people who may be nearby.
- Don't hold the person down or try to stop their movements.
- Time the seizure.
- Clear the area around the person of anything hard or sharp.
- Loosen ties or anything around the person's neck that may make breathing difficult.
- Put something flat and soft, like a folded jacket, under the person's head.
- Turn them gently onto one side. This will help keep their airway clear.
- Do not try to force their mouth open with any hard implement or with fingers. A person having a seizure CANNOT swallow their tongue. Efforts to hold the tongue down can injure teeth or the jaw.
- Don't attempt artificial respiration except in the unlikely event that a person does not start breathing again after the seizure has stopped.
- Stay with the person until the seizure ends naturally.
- Be friendly and reassuring as consciousness returns.
- Offer to call a taxi, friend or relative to help the person get home if they seem confused or unable to get home by themself.
Most generalized tonic-clonic (grand mal) seizures end by themselves. In a person with a history of seizures, they are not a medical emergency even though they can appear frightening. If the seizure stops naturally after a few minutes without injury, the person does not necessarily need to go to a hospital. In other circumstances, an ambulance might need to be called.
An ambulance should be called if:
- The person does not have a history of seizures.
- The seizure happened in water.
- The person is not wearing any medical ID, and there is no way of knowing whether or not the seizure is caused by epilepsy.
- The person is pregnant, injured, or diabetic.
- The seizure continues for more than five minutes.
- A second seizure starts shortly after the first has ended.
- Consciousness does not start to return after the shaking/convulsing has stopped.
If the ambulance arrives after the person has returned to consciousness, the person should be asked whether the seizure was associated with epilepsy and whether emergency care is needed.
What are some of the causes of epilepsy?
There are many causes of epilepsy. Some causes are hereditary and can results in seizures starting in either childhood or as an adult. Other causes include head trauma, meningitis, brain tumors, stroke, or multiple sclerosis. However, if you have experienced a seizure, please note that many times, none of these diagnoses are made. In most cases, no clear cause of the seizure can be determined. Please consult with you physician about your personal situation.
How is epilepsy diagnosed?
Epilepsy is diagnosed by meeting with your neurologist and undergoing a series of basic tests. The first step is to review your medical history (including a detailed recounting of the seizures) with your physician. This physician will also conduct a thorough neurological examination. In most cases, an EEG (electroencephalogram) and MRI (magnetic resonance imaging) test will be performed as well. You will meet with the physician after these tests to discuss your overall personal health situation.
How is epilepsy treated?
The mainstay of epilepsy therapy remains anti-seizure medications. Various medications have been used for decades, and they remain very effective for the majority of patients with epilepsy. In more recent years, medications with better side effect profiles and safer long-term records have been introduced.
For patients who do not respond to medications, the vagus nerve stimulator and respective epilepsy surgery are also options. Finally, there are a number of investigational interventions currently in development. Please discuss these options and your personal situation with your neurologist.
What is an electroencephalography (EEG)?
![]() An electroencephalogram (EEG) is a test to detect abnormalities in the electrical activity of the brain. Brain cells (or neurons) communicate by producing electrical signals. To perform an EEG test, electrodes are placed on the scalp to detect and record patterns of this electrical activity and check for abnormalities.
An electroencephalogram (EEG) is a test to detect abnormalities in the electrical activity of the brain. Brain cells (or neurons) communicate by producing electrical signals. To perform an EEG test, electrodes are placed on the scalp to detect and record patterns of this electrical activity and check for abnormalities.
The test is performed by an EEG technician in a specially designed room that is located in the hospital. At the beginning of the test, you will lie on your back on a table or in a reclining chair. The technician will apply between 16 and 25 flat metal discs (the electrodes) in different positions on your scalp. The electrodes are affixed to your scalp with a paste and are connected by wires to an amplifier and a recording machine. There is no invasive part of this test, and you should feel no discomfort.
As the test begins, the recording machine converts the electrical signals into a series of wavy lines that are recorded on a computer. You will need to lie still with your eyes closed because any movement can alter these results. You may be asked to do certain things during the recording, such as breathe deeply for several minutes or look at a flickering light.
Your health care provider may want you to discontinue some medications before the test. Do not change or stop medications without first consulting your physician.
You should avoid all foods containing caffeine for 8 hours before the test.
Sometimes it is necessary to sleep during the test, so you may be asked to reduce your sleep time the night before. Please discuss this possibility with your physician.
The EEG test is used to help diagnose the presence and type of seizure disorders, to look for causes of confusion, and to evaluate head injuries, tumors, infections, degenerative diseases, and metabolic disturbances that affect the brain. It is also used to partly evaluate sleep disorders and to investigate periods of unconsciousness.
What is Magnetic Resonance Imaging (MRI)?
An MRI (magnetic resonance imaging) scan is a non-invasive procedure that uses powerful magnets to construct pictures of the body. Unlike conventional radiography, which uses potentially harmful radiation (X-rays), MRI imaging is based on the magnetic properties of atoms. A powerful magnet in the machine generates an intense magnetic field around the body, and some hydrogen atoms within the human tissue will align with this field. When radio wave pulses are directed at this tissue, the hydrogen atoms that have been affected by the magnet will return a signal. These signals are used to construct pictures of the part of the body being examined. In the case of epilepsy, the brain is the subject of interest.
The MRI scanner must be located within a specially shielded room to avoid outside interference. The patient will be asked to lie on a narrow table which slides into a large tunnel-like tube. If contrast is to be administered, an IV will be placed, usually in a small vein of the hand or forearm. A technologist will operate the machine and observe you during the entire study from an adjacent room. Several sets of images are usually obtained, each taking from 2 to 15 minutes. A complete scan may take up to one hour or more.
No preparatory tests, diets, or medications are usually needed before having an MRI performed. An MRI can be completed immediately after other imaging studies. Because of the strong magnets, certain metallic objects are not allowed into the room. Items such as jewelry, watches, credit cards, and hearing aids can be damaged, and must be removed prior to taking the test. Removable dental work should be taken out just prior to the scan. Pens, pocketknives, and eyeglasses can become dangerous projectiles when the magnet is activated and should not accompany the patient into the scanner area.
Because the strong magnetic fields can displace or disrupt the action of implanted metallic objects, people with cardiac pacemakers cannot be scanned and should not enter the MRI area. MRI also should not be used for people with metallic objects in their bodies, such as: inner ear (cochlear) implants, brain aneurysm clips, some artificial heart valves, older vascular stents, and recently placed artificial joints. Sheet metal workers, or persons with similar potential exposure to small metal fragments, will first be screened for metal shards within the eyes with X-rays of the skull.
The patient will be asked to sign a consent form confirming that none of the above issues apply before the study will be performed. A hospital gown may be recommended, or the patient may be allowed to wear "sweats" or similar clothing without metal fasteners.
There is no pain experienced during the scanning procedure. However, some people do have a claustrophobic. The table may be hard or cold, but you can request a blanket or pillow. The machine produces loud thumping and humming noises during normal operation. Ear plugs are given to the patient to reduce the noise. For people that have trouble with small spaces, a mild sedative may be used during the scan. If this is done, someone needs to be available to help get the patient home.
A technologist observes the patient during the entire procedure and may speak through an intercom in the scanner. Some MRI scanners are equipped with televisions and special headphones to help the examination time pass.
What is a Positron Emission Tomography (PET) scan?
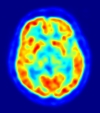 A Positron Emission Tomography (PET) scan is a diagnostic exam that evaluates the energy activity of the brain. Positrons are tiny particles released from a low dose of radioactive substance administered to the patient prior to the exam.
A Positron Emission Tomography (PET) scan is a diagnostic exam that evaluates the energy activity of the brain. Positrons are tiny particles released from a low dose of radioactive substance administered to the patient prior to the exam.
The PET scan measures how intensely different parts of the brain use up glucose, oxygen, or other substances. A small amount of a radioactive substance is injected into one of the patient’s veins prior to the test. This substance attaches itself to glucose. Small objects (positrons) are released from the tagged glucose, which is detected by the PET scanner. The images that result are helpful in diagnosing a variety of conditions and diseases, including epilepsy.
The PET images are programmed to show different colors or levels of brightness. The possible area where a seizure occurs may appear darker in the brain tissue in comparison to other areas.
The actual PET scanner looks like a large doughnut. Around the central hole of the machine are rings of detectors that record the emission of positrons. As the patient lies on a cushioned table, the patient will be moved into the central hole of the machine. The test will take about 90 minutes. The patient should not eat for at least 6 hours before the PET scan. The patient will be encouraged to drink several glasses of water before the test.
The PET scan itself will cause no discomfort. The patient will lie in a cushioned examination table and be asked to remain still during the exam. Some patients who are claustrophobic may feel anxious while positioned in the PET scanner. Patients should talk with their physicians if they have a history of claustrophobia.
The PET scan allows physicians to better evaluate the functioning of different regions of the brain. It can show where seizures potentially start and help determine if a patient is a candidate for surgery.
For pregnant and nursing women, the radioactive substance may expose the fetus or infants who are breast-feeding to a small amount of radiation. The risk to the fetus or infant should be considered in relation to the potential information gained from the result of the PET examination. If the patient is pregnant or may be pregnant, the patient should inform the PET imaging staff before the examination is performed.
What is Video EEG Telemetry?
Inpatient video EEG monitoring enables the physicians to gather additional information about the specific types of seizures patients are having. The more accurately we are able to classify the seizure type, the better the chances are to achieve seizure control with medications.
Additionally, for people who are having spells without a clear diagnosis, video EEG telemetry can often be useful in characterizing such episodes. These spells may be diagnosed as epileptic seizures, but may also be determined to be psychogenic non-epileptic events, syncope, or cardiac-related spells.
Video EEG telemetry also assists physicians in localizing the seizure focus in the brain. This is critical if patients wish to know if they have the type of seizures that may be treated surgically. Seizure surgery is most successful when physicians are able to localize the precise area in the brain where seizures originate. Prolonged video EEG monitoring allows physicians to record a number of seizures, providing the best video and EEG data possible
The video EEG telemetry procedure has two parts:
1, EEG Telemetry: As during a routine EEG, electrodes are glued to the patient’s scalp. The electrodes then record for 24 hours per day. A computer monitors the EEG recording continuously so that seizure activity can be marked. This recording gives physicians an accurate count of seizures and allows the doctors to compare what is physically happening to the patient during a seizure with what is seen on the brain wave recordings.
2, Video: A camera is used to continuously film the patient while you are connected to EEG electrodes. By using the video, the physicians can see what happens to patients physically while they are having a seizure. Seeing what happens physically allows the physicians to better determine what type of seizures the patient is experiencing and where the seizure might be starting in the brain.
What is Magnetoencephalography (MEG)?
A magnetoencephalogram (MEG) is a test that identifies brain activity by measuring small electrical currents arising from the neurons of the brain. These currents produce magnetic fields. The MEG generates an accurate location of the magnetic fields produced by the neurons. The MEG test is somewhat related to the electroencephalography (EEG) test except that it is using magnetic fields as the primary information for determining where seizures might be originating.
The MEG test takes approximately two hours. An EEG is done at the same time as the MEG. Electrodes will be placed on the patient’s scalp using paste. All electronic items or items with a magnetic strip (cell phones, credit cards) will be removed. Also, all metal above the waist should be removed, such as under wire bra, shirts with zippers or snaps, jewelry and wrist watches. The patient will be in a specially shielded room during the test, and will lay in a bed with the head resting in the helmet-like MEG scanner. The MEG scanner does not emit radiation or magnetic fields. It only detects and amplifies magnetic signals produced by the brain.
There are video and intercom systems in the room. The technician can see, hear, and communicate with the patient at all times. During the scan, the patient must keep his/her head still. The head is immobilized by using cushions that are placed on both sides of the head.
The patient may be asked to arrive sleep-deprived in the hopes of recording brain activity in the awake, drowsy, and sleep states.
The MEG test causes no discomfort. The scanner does not make noise. The patient will be able to have someone in the room with you during the test, but they must also remove electronic and metallic objects.
About Pre-surgical Evaluation for Epilepsy
Many patients have similar questions about having seizure surgery and what tests may be needed before surgery. The following general information is intended to provide some answers. However, each epilepsy patient is unique and his or her care is always individualized. All patients should discuss their unique situation with their physician.
Seizure surgery is an operation aimed at removing the area of your brain that is causing the seizures. The goal of surgery is to improve seizure control and when possible, to stop seizures completely. There are several types of seizure surgery, and every patient is approached as a unique individual.
After several medications have failed to control a patient’s seizures that individual’s epilepsy is called refractory. Studies have shown that in cases of refractory epilepsy, medications are less likely to work. Surgery may help some of these patients, and seizures may come under control with the addition of surgery. For patients who are open to this option, a surgical evaluation may be initiated.
Results from the video EEG telemetry session give the doctors a better understanding of what part(s) of your brain the seizures may be arising from. If most of the seizures are coming from one specific area, it may be possible to safely remove this area (seizure focus) in an effort to control the seizures. However, there are additional tests that will be needed in order to help the epilepsy team determine exactly where the seizures arise from and whether surgery is a safe option.
The full epilepsy team consists of epileptologists (doctors specializing in epilepsy), brain surgeons (neurosurgeons), radiologists, neuropsychologists, an epilepsy nurse, a neurosurgery nurse practitioner, the EEG technologists, and the scheduling staff.
There are several types of additional tests that may be needed before being considered for surgery. Some of the tests include: Magnetic Resonance Imaging (MRI), Positron Emission Tomography (PET), Magnetoencephalography (MEG), Neuropsychological testing, and the Wada test.
The information gathered from the tests above is aimed at better defining and localizing your specific seizure focus and to help determine if that focus can be safely removed.
In some cases, however, the results of the tests may give the epilepsy team an idea as to where the seizures start but not enough information to be conclusive. If the initial scalp EEG or radiological testing doesn’t provide enough localizing information, the patient may need further evaluation using intracranial monitoring (Invasive Monitoring). Intracranial monitoring records brain wave activity using electrodes placed surgically in or on the surface of the brain.
If surgery is found to be an option, the last two tests are the neuropsychological evaluations and the Wada test. The neuropsychological evaluation will be done by a neuropsychologist. Extensive testing may determine the site of the seizures, as well as appraise the possible effects of the surgery on cognitive functioning.
The Wada test evaluates the location of speech and memory functions in the patient’s brain. This test is done in an angiography suite with the radiologist, neurologist and anesthesiologist. Sodium amytal, a short acting medicine, will be used to sedate one side of the brain while the other side is being tested by a neuropsychologist. The results of this test determine which side of the brain is the dominant area for crucial functions, such as language. It may determine whether the patient will be awake during part of the surgery. This test and its results should be discussed with the patient’s physician in detail.
Once the Epilepsy Team has obtained and reviewed all the necessary tests, they will present the results to the patient and together, the patient and physician team will make a decision about surgery.
What is Invasive Monitoring?
Invasive monitoring is a term that refers to recording brain waves using electrodes placed in or on the surface of the brain. In rare cases when scalp recordings do not localize your seizures, intracranial electrodes may be necessary to acquire further information. This procedure involves undergoing surgery to place the electrode at various places on the surface of the brain. These electrodes allow your physicians to get much higher quality information that what normal scalp-based electrodes can detect.
Ultimately, your physicians will determine if you are a candidate for having intracranial electrodes. In almost all cases, this is an advanced test that is only performed for patients who are being considered for epilepsy respective surgery.
If this decision is made, the epilepsy team will determine the number, the type and the exact placement of electrodes needed to further evaluate the seizure focus. There are different types of intracranial electrodes, including depth electrodes, subdural strips, and subdural grids all of which are placed by the neurosurgeon. You will get details about your particular situation if this intervention becomes necessary.
If you have this procedure, you will be admitted to the hospital at least a day before the placement of the intracrainal electrodes. You will need to wash your hair the night before the procedure. Part of your head will likely be shaved. This is done to prevent infection. Plan to stay in the hospital for at least 5 to 7 days after the electrodes are placed. After the electrodes are placed, you will be in a private monitored room such as the one you were in for video-EEG recordings. The overall test is very similar to routine video EEG monitoring, except that the electrodes are invasive.
You may experience scalp pain and headaches after the procedure. You may also experience some scalp or face swelling, especially with a grid set of electrodes. Your nurses and doctors will do all they can to make you comfortable.



















